How can we embed and spread the positive changes emerging through coronavirus (COVID-19)? How do we identify those innovations that will be useful longer term, whether or not they’ve emerged recently? How can we ensure there’s sufficient evidence behind the things we scale? Where should we focus to have the biggest benefit for the population without our capacity for supporting roll out properly being (ahem) spread too thin?
Q brought together our partners – leaders from the national improvement teams across the UK and Ireland – to explore this strategic challenge last week. We know from workshops Q is running that capturing and selecting changes to embed is a priority shared by many at all levels in the health and care system. This blog summarises key insights from the call that I believe can unlock a more coherent approach, whether you’re thinking about this across your organisation, region or country.
Look for pre-COVID innovations whose time has come
The language of innovation can disguise the fact that many of the changes coming to the fore during COVID build on an established rationale and evidence base
The language of innovation can disguise the fact that many of the changes coming to the fore during COVID build on an established rationale and evidence base. Drawing on the work of Walter Schiedel, Ruth Glassborow, Director of Improvement in Healthcare Improvement Scotland, explained ‘there are changes we’ve needed to make in health and care for some time, that are now gaining traction and becoming more possible thanks to the different context of COVID. This is about both big ideas about how we organise health and care (such as the need to rely less on services and do more to support self-management and community-led responses) and specific service innovations (such as models for hospital at home or remote monitoring)’.
Understand the mindset shifts enabling these innovations
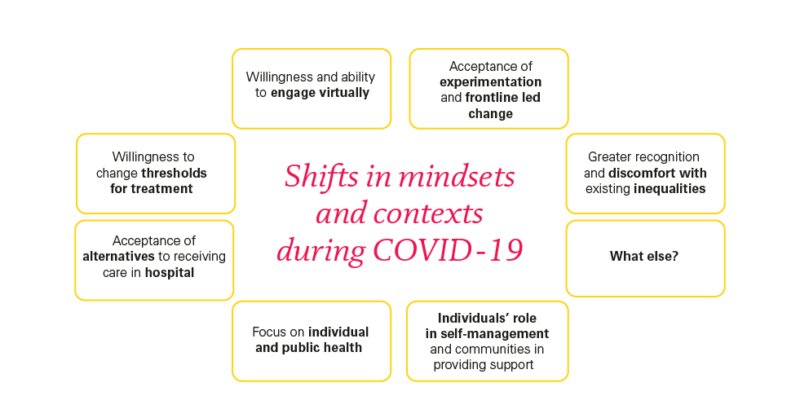
So, what are the big ideas that appear to be gaining particular momentum during COVID? Especially while the pandemic, and NHS and public responses to it, continue to evolve, it’s hard to be definitive. However, building on discussions within Scotland, we identified seven key areas where a different context has prompted new attitudes and action that seem broad and deep enough to suggest at least a temporary shift in mindset.
- Willingness and ability to engage virtually
- Acceptance of alternatives to receiving care in hospital
- Willingness to change thresholds for treatment
- Recognition of individuals’ role in self-management and communities in providing support
- Focus on individual and public health
- Greater recognition and discomfort with existing inequalities
- Acceptance of experimentation and front line-led change
How these insights can help us keep and spread positive changes
Paying attention to the evidence base and to broader shifts in mindset and context that lie behind innovations can highlight which changes are most likely to be ready to spread and deliver systemic benefits for patients and population. It could also help with developing ways to communicate and embed these changes – getting beneath the practicalities to also connect with the underlying beliefs and assumptions influencing uptake by both clinicians and the public. This opens up a more transformational understanding of the change we’re going through.
Through giving it a go, often through necessity, both clinicians and service users have often been surprised by what is possible
Video consultations illustrates this well. A service change with an evidence base and policy consensus built through inching progress over a decade, uptake has dramatically increased during COVID, thanks to changes in context and alignment with several of the mindset shifts above.
Through giving it a go, often through necessity, both clinicians and service users have often been surprised by what is possible, with mindsets thereby evolving about risk and the contexts within which video consultations might be appropriate.
The debate we’re seeing about how far this should go is connected to broader questions about accessibility, equality and the clinician-patient relationship – with engagement best when we recognise this as far more than a ‘surface’ change to processes.
Join the conversation: What mindset shifts do you see? How might this help our work?
I believe the idea of shifts in the mindsets and conditions for service change can be really helpful as we think about spread, and so I’d expect it to provoke discussion. On the call, we started to explore some of the questions this raises.
I believe the idea of shifts in the mindsets and conditions for service change can be really helpful as we think about spread
What are the mindset shifts to pay attention to? When we talk about mindset shifts, what do we really mean and how might we sense and measure such shifts? Which voices are amplified and which are muted as we think about this? Where are new norms being formed now that traditional spaces are being replaced by online mechanisms for sense-making and debate?
As we get a clearer view of the shifts, how will we know which will last? What might swing back when an exhausted workforce and population see an end to the current crisis phase of the pandemic? What do we need to do now to get on a helpful course, recognising a limited window of opportunity before the potentially overwhelming pressures of recovery? How do we attend to shifts that might be less positive, such as over-reliance on command and control, top-down leadership?
When we think about specific change ideas linked to these shifts, how do we judge how much evaluation or assurance is needed? How might we think broader about innovation ideas that haven’t yet come to the surface, but might be critical to our new normal? How can we approach sustainability and spread in a way that recognises and engages with the interwoven and ongoing changes to context, process and mindset?
It would be great to hear your thoughts: add your comments below, or share your thoughts with us on Twitter. This resonated with those working at a national level across the UK and Ireland; does it resonate with you? What might we be missing?
Q is regularly bringing together leaders from the national improvement organisations across the UK and Ireland. You can read about the first COVID discussion in this summary blog from Penny.
Comments
Carolyn Jackson 3 Jun 2020
Our work on the Venus model may be useful to the Q Community on thinking about an integrated approach to systems transformation work.
Karen Fechter 4 Jun 2020
Hi Caroline
Sounds interesting. I can see on your Q bio that you've recently published a paper on the Venus model. Is it available free to access or would you be able to share a copy?
Carolyn Jackson 4 Jun 2020
Hi Karen if you email me I can send it to you as a file attachment carolyn.jackson1910@gmail.com
Penny Pereira 8 Jun 2020
Hi Caroline, Thanks for flagging this. The Venus model includes a lot of rich information about how to approach service transformation. Are there particular stems or practices that you think are particularly coming to the fore during covid? How might the current context influence the strategies that are needed and will work?