At the Q Community event last month, I proposed three priorities for increasing the impact of the work we do individually and together to improve health and care. The recording of the live stream is now live on the Q website.
I blogged a few days later to explain what Q will be doing in each of these three areas over the months and years ahead. In this blog, I wanted to share some of the top sources that have influenced our thinking and the theory of change for Q.
This three-part vision for a more collaborative approach to improvement is an attempt to distil key themes from the work of the Foundation, our partners, and relevant literature, and bring that together with what we’re learning from the Q community. Here’s a selective list of published sources we’ve found most interesting in this territory. Do tell us what you’d add into the mix: whether it reinforces, refines, or should make us revisit how we’re thinking about this.
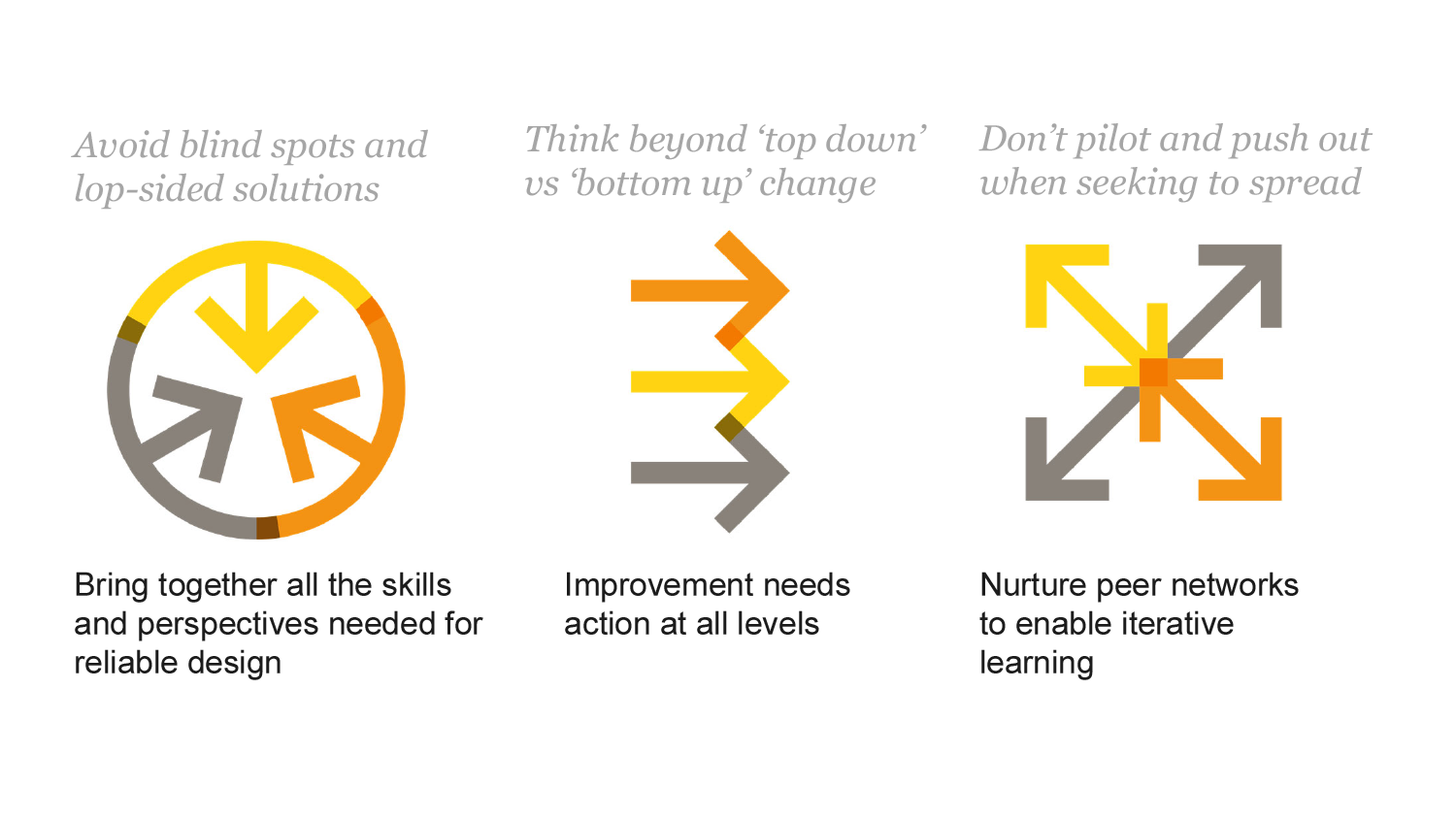
Bringing together all the skills and perspectives needed
We need to be able to tap into a range of different skills and perspectives to understand and deliver even relatively straightforward change well. Especially when time and resources are tight, we tend to over-rely on those people and techniques we have most readily to hand. But this can risk solutions being ‘lop-sided’, lacking the robustness or buy-in that will allow them to thrive long term.
Safer clinical systems evaluation observes how frontline teams often jump to action, and how ideas can be generated from the perspective of particular staff groups, neglecting other perspectives.
Overcoming challenges to improving quality describes eloquently the different skills that improvement needs to draw on. As does Skilled for improvement.
Getting more health from healthcare: quality improvement must acknowledge patient co-production, makes the case that health care is inherently co-produced with service users and that they need to be more integrated into improvement. Engaging patients to improve quality of care: a systematic review identifies strategies and contextual factors that enable optimal engagement but concludes that more evidence is needed to understand patients’ experiences of the engagement process itself.
The challenge and potential of whole system flow argues we need to we bring together perspectives and skill up people from all organisations across a system if we’re going to achieve ambitions for redesign.
The Big Room methodology developed within Lean and now spreading wide as part of the Flow Coaching Academy provides a methodology for bringing multiple perspectives together to make progress on service design challenges.
Aligning action at all levels in the system
We know that the organisational and system context we’re working in makes a big difference to the success of improvement efforts. Current incentives, culture, budget choices and other factors can get in the way of the change we need to see at the frontline.
the organisational and system context we’re working in makes a big difference to the success of improvement efforts
What’s the solution? I see approaches to change that start centrally but feel disconnected from the mainstream reality of the services they are seeking to affect; sometimes getting stuck in structural shifts rather than being rooted in what will make a difference at the point of care or fizzling out once the central push and support moves on. Then there are other approaches from the bottom up, generating huge enthusiasm but also struggling to embed long term. The Health Foundation’s work suggests that complex change typically needs action at all levels.
Does Quality Improvement Improve Quality? Articulates the tendency of QI to ‘let a thousand flowers bloom’ and calls for action to be taken at the right level in the system.
The Health Foundation’s thinking on context underpins the calls we make on the national level to support change in a different way. Constructive comfort: accelerating change in the NHS outlines factors related to leadership, management, culture and data that are needed to support change across all levels in clinical teams, providers, commissioners and at the national level.
Mary Dixon Woods and Michael West describe in their paper Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study the ‘priority thickets’ of multiple and sometimes conflicting imperatives that can confuse action.
A different approach centrally could make space for local organisations and systems to develop and mature organisation-wide approaches to improvement, as described in The improvement journey.
Both nationally and locally, developing Quality Management Systems can support a more joined up and coherent approach to enabling high quality care. The work Scotland has done provides useful insight for others.
#NewPower ideas have been shared widely within the NHS through the NHS Horizons team and Helen Bevan, whose work is cited in the book. This is both challenging conventional ‘top down’ mechanisms, while describing the need to bring together both old and new power tactics to achieve change.
Nurturing peer networks to enable iterative learning and spread
We must get much better at ensuring what we learn is reliably taken up everywhere that can benefit
The implication of the two priorities above are that we need to invest more time in developing an understanding of issues and potential solutions and in working out what this means at the frontline, organisation and system level. Given the urgency and scale of the challenges facing the health sector, and the pressure on resources, we must get much better at ensuring what we learn is reliably taken up everywhere that can benefit. We know that the ‘pilot and push out’ strategies that we often reach for now aren’t working reliably. Peer networks are only part of the solution, but an important part.
The Health Foundation’s work on spread including the reports Against the Odds and The spread challenge, outlines the need to shift emphasis towards adopters, referencing the role that networks can play in supporting spread.
The Health Foundation’s Scaling Up Improvement and Exploring social franchising and licensing programmes are demonstrating strategies for spread better designed to maintain impact even as an idea is expanded to new settings.
Trish Greenhalgh’s book Implementing Evidence Based Medicine, articulates well the role of networks in generating and sharing knowledge and spreading innovation, with relevance to wider service change.
Effective Networks for Improvement describes five key features of effective networks – common purpose, cooperative structure, critical mass, collective intelligence and community building.
The Health Foundation’s Closing the gap through Clinical Communities programme evaluation outlines more on the characteristics of effective networks, with the NHS Improvement Source4Networks site including a range of practical resources for networks.
The world of thinking and practice in improvement is vibrant and evolving fast. What would you add to this list? Please reply to this blog, with what you think evidence and practice is telling us in these areas.
Comments
Thomas John Rose 14 Dec 2019
I'm encouraged by your mention of Quality Management Systems. An important feature of a good Quality Management System is implementing a Process Approach. This approach would greatly enhance all the QI activity undertaken in the NHS and which is encouraged by Q.
Penny Pereira 17 Dec 2019
Thanks Thomas, did you catch the Q Visit to Scotland focused on QMS or the webinar with Hugh McCaughey? - future plans for improvement in the NHS in England are drawing heavily on these ideas too.
https://q.health.org.uk/event/visit-to-healthcare-improvement-scotland-sustaining-improvement-through-quality-management-systems/